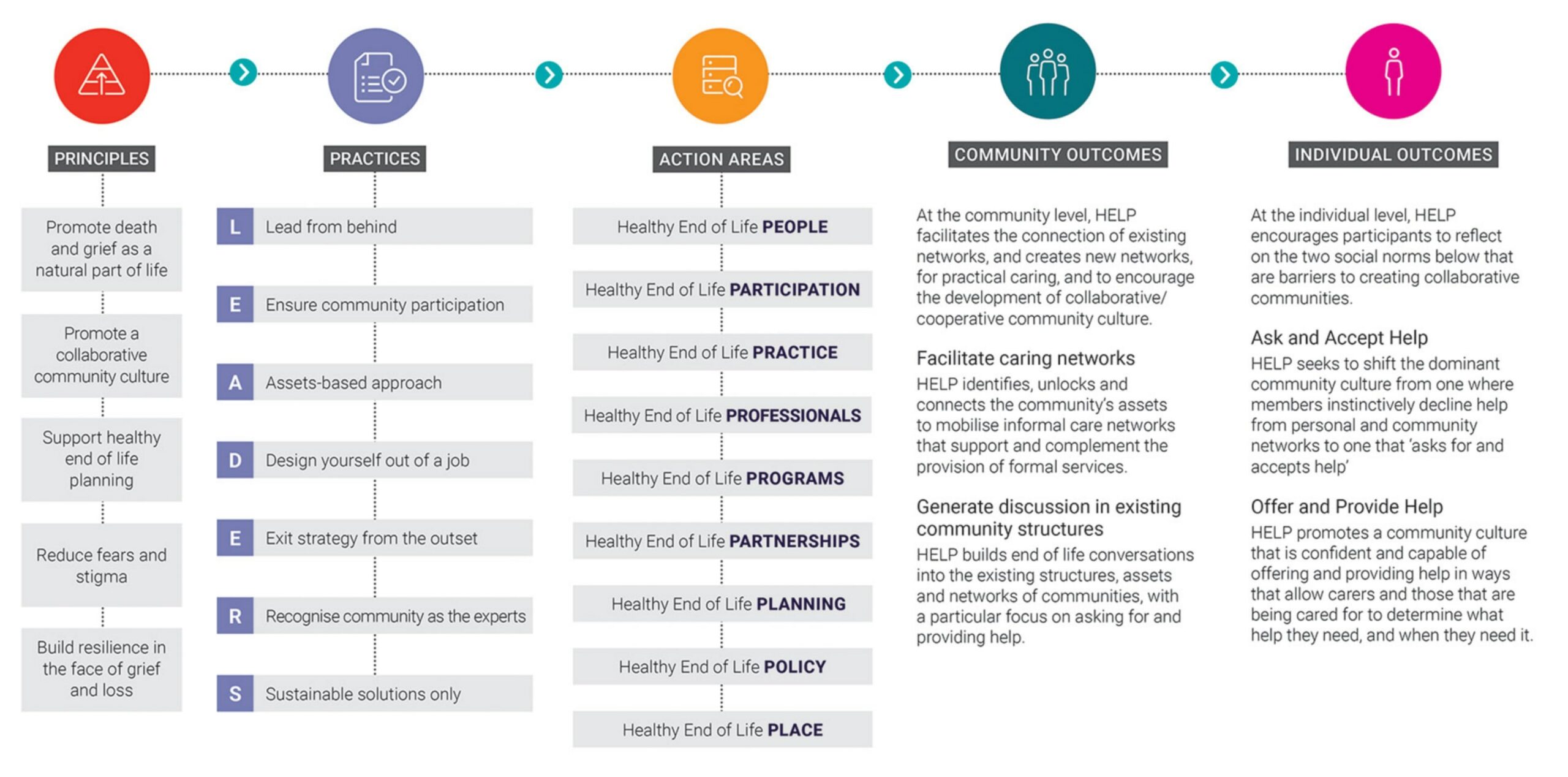
Overview of our HELP framework
Unlocking individual and community support networks through health and community sector partnerships.
Program objectives
HELP is a best-practice framework for implementing and evaluating population-level interventions in the public health sector.
Individual capability without public messages about shifting community culture limits the growth of collective action, while community awareness alone will not necessarily translate into practical caring networks that support homebased dying. Both are needed.
– Grindrod A., Rumbold B. 2018
By contributing to an integrated end-of-life care system, HELP seeks to enhance end-of-life’s social dimensions. And link these with the medical dimensions needed to support Australians nearing the end of their lives.
The Healthy End of Life Program (HELP) takes a research-informed approach. Based on strengths and assets, HELP is grounded in evidence-based health promotion strategies.
To facilitate change and impact, HELP aims to influence:
- Individual systems
- Community systems
- Service and organisational systems
- Policy systems and settings (location or place-based interventions)
At grassroots level, HELP’s approach supports Australians approaching the end of their lives. It enables them to remain connected to the people, places and possessions most important to them, and receive the right help – at the right time.
With the HELP framework, we aim to develop a public health palliative care approach. One where end of life is everyone’s responsibility – and everyone can play a role. One that empowers individuals and communities to act in new, constructive ways. And, cooperatively, generate pathways for end-of-life care in community- and home-based settings.
The HELP Palliative Care Social Prescribing Service model; The HELP Brief Intervention and the HELP App are all built around this evidence-based HELP framework.

Culture
- Shift community culture around death and dying
- Shift social norms around offering and accepting help
- Change practice and attitudes towards palliative and end-of-life care

Capacity
- Increase capacity around death, dying, loss and care
- Support those who wish to receive palliative and end-of-life care at home, or home-like settings
- Provide support that complements that of existing formal services
- Sustain carers within home or community-based settings

Collaborative communities
- Ensure the inclusion of those facing illness, ageing, frailty or loss
- Promote discussion and development of social care networks
- Encourage new and constructive action towards palliative and end-of-life care
Key research findings
What does the research tell us?
People didn’t ask for help
Despite carers’ existing support networks of family, friends and neighbours, asking for help was not considered an option, even when it was clearly needed. Requesting increased support from formal services was perceived as an easier and more acceptable alternative.
People didn’t accept help
Almost without exception, carers were either reluctant to accept help or declined help when it was offered by friends and family. In these instances, refusing support was overwhelmingly described as an instinctive response made without considering the value or necessity of the assistance. When participants were asked why they refused help, the three most common responses were to avoid ‘being a burden’, because dying was a ‘private matter’ and because ‘needing support’ was perceived as ‘not coping’, and therefore socially unacceptable.
People didn’t offer help
Participants in extended support networks and broader community networks reported that their willingness to offer help or support was hindered by uncertainty about the appropriateness of their proposed assistance. They were also hesitant to infringe on others’ privacy, echoing the carers’ sentiments that dying is a private matter.
People want to help
Participants shared a concern about the low understanding of palliative and end-of-life care within their community. Encouraging individuals to acknowledge their vulnerability and to ask for help was seen as an effective strategy to support local people during times of need.
When help becomes unhelpful
To create a healthy collaborative community culture around asking for and accepting help, it was imperative that the person and their carer retained control and autonomy over exactly what that help and support looked like. It was up to the community to establish from the outset and make explicit what this culture entailed and how the desired social norms could be upheld without causing conflict. Carers were more likely to accept help when the community culture supported them in maintaining their boundaries to prevent unwanted intrusive behaviour from often well-meaning helpers.

Revisiting social norms
The findings demonstrate that social norms about helping may be a significant barrier to creating a collaborative
community culture, which has implications for public health approaches to palliative and end of life care.
A public health practice model must modify these social norms if community capacity is to be mobilised effectively.
HELP seeks to shift current attitudes and perceptions by directly addressing the social norms of offering, accepting
and asking for assistance.

Rethinking independence
Identifying as someone who requires and requests support can make people feel vulnerable. Whilst some experience a
loss of independence and control as a loss of autonomy, the reality is that interdependence is inherent in communities.
Learning to accept this interdependence is a skill that sustains autonomy during periods of vulnerability and is often
developed through first providing support to others.
HELP facilitates this exchange as community members are encouraged to offer their support to others at a time of need. In addition to the value of the support offered at the time, there is a longer-term benefit for those who offer support and learn to engage constructively with their own vulnerability.

Involve the community
All those who participated had a genuine desire to provide care to members of their community at the end of life.
However, this desire was undermined by a shared perception that enquiring about community members’ support needs
as they neared the end of life might breach their privacy.
HELP contends that end-of-life care is everybody’s business, that end-of-life matters should be incorporated into existing community networks, and that gaps that are identified should be seen as opportunities for developing new initiatives.
Help outcomes
What changes occur when the HELP framework is applied
HELP is the product of ongoing research commencing in 2016, seeking an answer to the question: What is involved in building individual capability and community capacity for palliative and end-of-life care?
The program aims, through community development strategies, to build end-of-life capacity and resilience in two strategic ways. It achieves this by:
Change two social norms
- Shift the culture from one where members instinctively decline help from personal and community networks to one that ‘asks for and accepts help’
- Reinforce and create a community culture that is confident and capable of offering and providing help.
Using two key strategies
- Generating community discussion on the role of community at end of life - through partnerships, community forums that promote public conversation and skill-sharing.
- Facilitating the development of social networks that can respond to individual and collective end-of-life care needs in the community.
HELP asks the question: how do we unlock individual and community support networks and, for those with few networks, where can social support be found?
Individuals
At the individual level, HELP encourages participants to reflect on the two social norms that are barriers to creating collaborative communities.
Ask and Accept Help
HELP seeks to shift the dominant community culture from one where members instinctively decline help from personal and community networks to one that ‘asks for and accepts help’.
Offer and Provide Help
HELP promotes a community culture that is confident and capable of offering and providing help in ways that allow carers and those that are being cared for to determine what help they need, and when they need it.
Communities
At the community level, HELP facilitates the connection of existing networks, and creates new networks, for practical caring, to encourage the development of collaborative/cooperative community culture.
Facilitate caring networks
HELP identifies, unlocks and connects the community’s assets to mobilise informal care networks that support and complement the provision of formal services.
Generate discussion in existing community structures
HELP builds end of life conversations into the existing structures, assets, and networks of communities, with a particular focus on asking for and providing help.
Evidence based framework
The HELP Framework
Using the HELP framework
As a HELP partner, you’ll have access to our full education and training program
We train professionals and community members to develop public health palliative care approaches to end-of-life care.
We offer: webinars, training and professional development and can provide co-branded resources to get you started.

HELP resources
Putting HELP into practice
Discover key resources for your HELP project.
Ready to start making a difference with your patients and carers?
Register your interest in becoming a HELP Provider
Gain access to our full education and training program, as well as exclusive resources to support your organisation to implement HELP Palliative Care Social Prescribing.

Ready to start making a difference?
Register your interest in becoming a HELP partner
Gain access to our full education and training program, as well as exclusive resources to support your HELP project – and measure your impact.